Know the Facts
What is a congenital heart defect (CHD)?
A congenital heart defect is a problem with the structure or functioning of the heart that is present at birth. Common examples include holes in the inside walls of the heart and narrowed or leaky valves.
How common are congenital heart defects (CHD)?
Roughly 40,000 children are born with a CHD in the US every year or approximately 1% (1 in 100). CHDs are the most common birth defects. CHDs are as common as autism and about 25 times more common than cystic fibrosis. Approximately 2-3 million people are thought to be living in the U.S with CHDs. Because there is no system to track CHDs beyond early childhood, more precise estimates are not available. Thanks to improvements in survival, the number of adults living with CHDs is increasing. It is now believed that the number of adults living with CHDs is at least equal to, if not greater that, the number of children living with CHDs.
Can you detect a CHD before birth?
A fetal echocardiogram can detect a CHD prenatally. A fetal echocardiogram is a test similar to an ultrasound that allows your doctor to better see the structure and function of your unborn child’s heart. It is typically done in the second trimester, between 18-24 weeks.
What is the health impact of congenital heart defects?
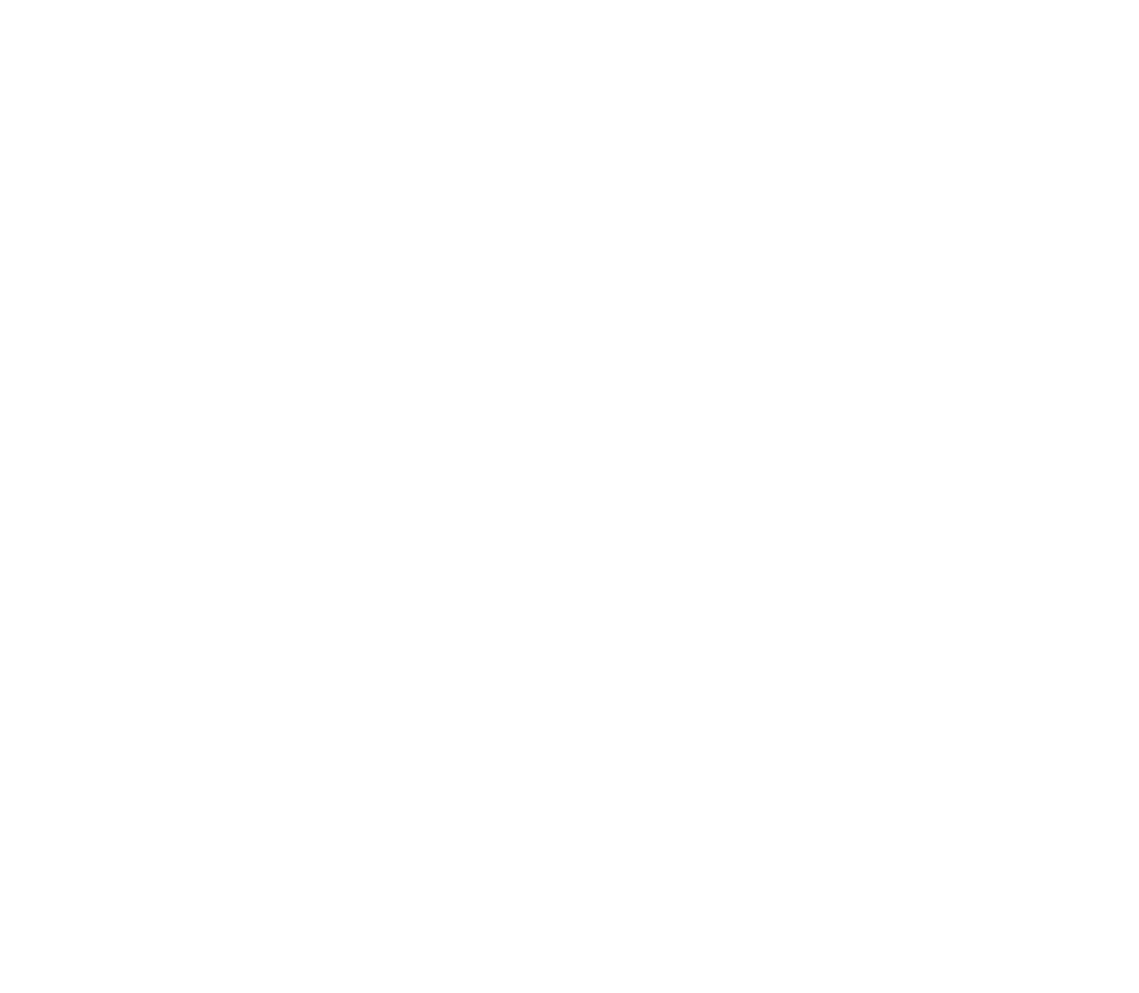
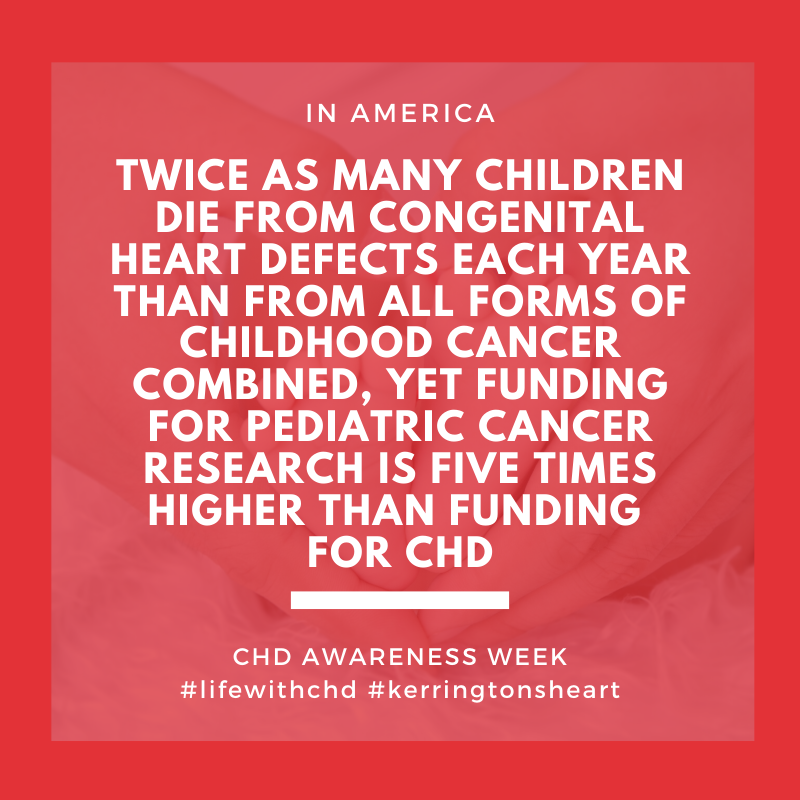
CHD’s are the most common cause of infant death due to birth defects. Approximately 25% of children born with a CHD will need heart surgery or other interventions to survive. Surgery is often not a cure for CHDs. Over 85% of babies born with a CHD now live to at least 18 years old. However, children born with more severe forms of CHDs are less likely to reach adulthood. Many individuals with CHDs require additional operation(s) and/or medications as adults. People with CHDs face a life-long risk of health problems such as issues with growth, eating, developmental delays, difficulty with exercise, heart rhythm problems, heart failure, sudden cardiac arrest or stroke.
What causes congenital heart defects?
The cause of most CHDs are unknown. Approximately 15% to 20% are due to known genetic conditions. Most CHD’s are thought to be caused by a combination of genes and other risk factors, such as environmental exposures and maternal conditions. Because the heart is formed so early in pregnancy, the damage may occur before most women know they are pregnant. Environmental exposures that may be related to risk of having a CHD include the mother’s diet and certain chemicals and medications. Maternal diabetes is a recognized cause of CHDs. Maternal obesity, smoking, and some infections also may raise the risk of having a baby with a CHD. Preventing these risk factors before a pregnancy is crucial. A baby’s risk of having a CHD is increased by 3 times if the mother, father, or sibling has a CHD.
What are the health care challenges related to congenital heart defects?
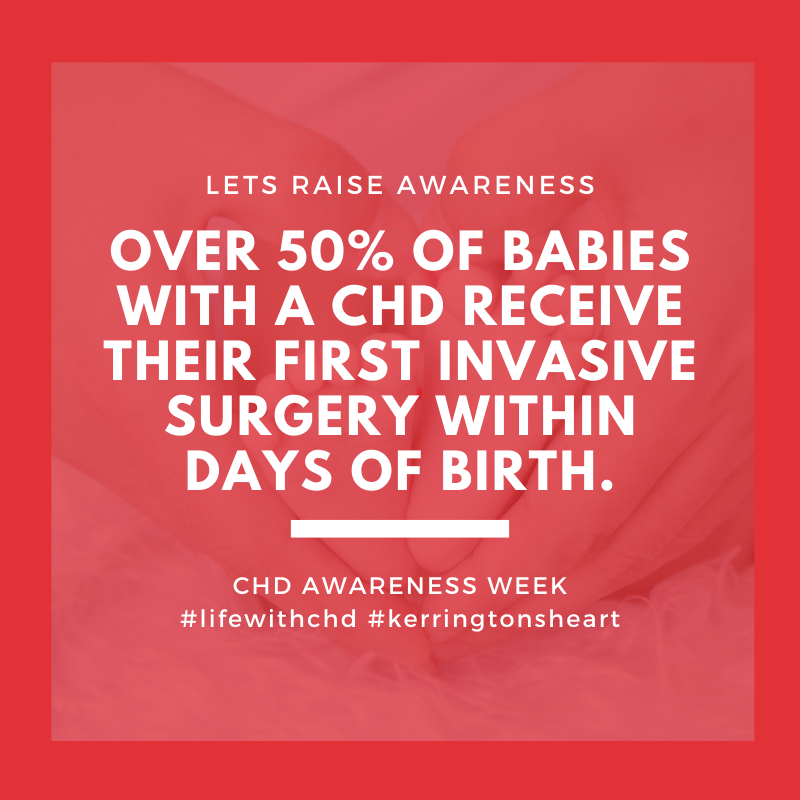
In 2009, the hospital cost for roughly 27,000 hospital stays for children treated primarily for CHDs in the U.S. was nearly $1.5 billion. In the same year, hospital cost for roughly 12,000 hospital stays of adults treated primarily for CHD was at least $280 million. A significant number of adults with CHD in the U.S. report having problems obtaining insurance and coverage for specialized care. Compared to the general population, adults with CHD have 3-4 times higher rates of emergency room visits, hospitalizations, and intensive care unit stays. Fewer than 10% of adults with CHDs in the U.S. who need care from specialty adult CHD centers are receiving this recommended care.
Reference: https://www.aap.org/en-us/Documents/chphc/chd_fact_sheet_short.pdf
Kentucky Newborn Screening
What is the Kentucky Newborn Screening Program and why is it important?
Pulse Oximetry is an initial screening tool for Critical Congenital Heart Disease (CCHD). Hospital administrators, birthing facilities, and medical personnel caring for newborns ages 28 days or less are required by law to assure that every infant in their care receives a pulse oximetry newborn test. The detection of CCHD’s increases to around 85% before hospital discharge with the use of a Pulse Oximetry as a part of an infants newborn screen.
Pulse Oximetry:
Measures the oxygen saturation of the blood;
Is non-invasive and painless;
Is accurate and reliable;
Is fast and easy to perform; and
Is inexpensive.
Pass
If the baby passes the screen (also called “negative” or “in-range” result), it means that the baby’s test results did not show signs of a low level of oxygen in the blood. A baby that passes the screen is unlikely to have a critical CHD. However, not all babies with a critical CHD will have a low level of oxygen in the blood that is detected during newborn screening. Thus, it is possible for a baby who passes the screen to still have a critical CHD or other CHD.
Fail
If the baby fails the screen (also known as “positive” or “out-of-range” result), it means that the baby’s test results showed low levels of oxygen in the blood, which could be a sign of a critical CHD. This does not always mean that the baby has a critical CHD but could mean that more testing is needed. There may be other causes, such as breathing problems, for low levels of oxygen in the blood. The baby’s doctor might recommend that the baby get screened again or have more specific tests, like an echocardiogram (an ultrasound picture of the heart), to diagnose a critical CHD.
For more information visit: https://chfs.ky.gov/agencies/dph/dmch/cfhib/Pages/newbornscreening.aspx
CHD vs CCHD
Knowing the difference between a CHD and a CCHD
A Congenital Heart Defect (CHD) is the most common congenital disorder in newborns.
Critical CHD, occurring in around 25% of those with CHD, is defined as requiring surgery or catheter based intervention in the first year of life. Listed below are 7 CCHD’s:
Hypoplastic Left Heart Syndrome (HLHS)
Tricuspid Atresia
Pulmonary Atresia
Tetralogy of Fallot (TOF)
Total Anomalous Pulmonary Venous Return (TAPVR)
Transposition of the Great Arteries (TGA)
Truncus Arteriosus
Other heart defects can be just as severe as these seven and also require treatment soon after birth. However, pulse oximetry screening may not detect these heart defects as consistently as the seven listed above.